Bmi vector created by svstudioart – www.freepik.com
This is the story of a number that’s come to haunt a lot of people and for no good reason.
And yet through the years, it’s been widely used as a weapon to induce guilt at your doctor’s office or in front of your personal trainer, and as an epidemiological signpost for disease risk, not to mention an actuarial determinant for life insurance policy sales.
It’s your BMI. The mathematical calculation of your weight in kilograms divided by your height in metres squared (kg/m2) that is known as the Body Mass Index.
Without knowing anything else about you and the habits you have or the race or sex you are or whether you are a body builder or a ballerina or someone with dangerously high levels of insulin, the BMI can slap a label on you that goes from underweight to normal to overweight, to obese, to severely obese, to super morbidly obese.
Because like a package to mail back to Amazon – what’s most important is to be able to divide your weight by your height.
Please.
It is high time we stopped thinking of ourselves as an Amazon package and quit allowing ‘professionals’ to rely on the BMI as the Holy Grail of health. This is a racist tool of shame, a lazy practitioner’s way of judging you and tells us very little, if anything, about health.
Let’s unwind this topic.
First, a little history
The BMI was developed about 200 years ago by a Belgian dude named Adolphe Quetelet. Was he a physician or involved in the study of medicine? Nope – he was an academic who’s strength was in statistics, astronomy and mathematics.
One of his key areas of study was to figure out the characteristics of the average man (not human, but man). He was fascinated by the regularity in statistical patterns and by documenting these, he believed society had a way to prove what the ideal population should represent.
What ideal was he striving for? Well, his formula was based on calculations made on only White Europeans. So consideration of body types from another race or culture was never even on the table.
I think you can see where the root of the issue began – in measuring an ideal against a narrow and specific standard for one thing. So racist, yes?
But it gets worse.
The morphing of the BMI as a measure of worthiness really began in earnest in the early 20th century when insurance companies started to compile tables of height and weight for the purpose of determining who might be too risky to insure. The tables were put together by actuaries and sales people, not medical experts, so how valid were they as any kind of health profile?
Remember – these companies had no more insight into a person’s overall health than how tall they were and how much they weighed in total. There was no accounting for body fat versus lean (muscle) tissue, so a fit and muscular railroad worker and a sedentary banker with a flabby physique and paunch who were the same height and weight might both come out as obese in the BMI. Or they might both come out as normal. Either way, the BMI measurement wasn’t really telling the story.
Keep in mind that these insurance tables were equally non-representative of a diverse population – as only the well-off, who could afford insurance, were logged into these algorithms used to determine who was a good bet for insuring.
And since women rarely bought insurance, their measurements were an afterthought. Another case of women being considered just mini-men as opposed to taking into consideration the fact that women’s bodies are composed of very different ratios of fat and lean tissues for good reason (hey, we’re baby-makers for one!).
Despite these shortcomings, doctors embraced these tables as a way to ‘diagnose’ and so the shaming of people for what they weighed began.
How the BMI and the rising obesity rate are intertwined
By the 1970s, the BMI had become fully entrenched as a diagnostic shortcut for obesity, thanks to Ancel Keys, a US public health bureaucrat, whose flawed Seven Countries Study set us off on a course of dietary fat as the biggest villain for raising cholesterol and contribution to cardiovascular disease. (Hint – this was a falsehood then and is a falsehood now.)
The study had many flaws – it was observational in nature and relied on self-reporting, which in itself is a red flag. I mean how many people are accurate in reporting what they eat and how much of it?
Additionally, one of the more egregious flaws included the fact that the data were cherry-picked from just seven of the 22 countries that participated (all of them White and mostly Euro-centric, except for Japan) thereby skewing the outcome.
There have been debunking and rebuttals over the year but regardless, the die was cast and North American nutritional guidelines shifted into low/no fat mode and made up the dietary gap by increasing grains and sugar.
By 1985, the National Institutes of Health (US) had firmly tied BMI to the pronouncement of a person’s status as obese. In 1998, the NIH shifted the definition and lowered the BMI scale and suddenly overnight millions more people were considered to be obese. (Fun fact: Canada followed suit.)
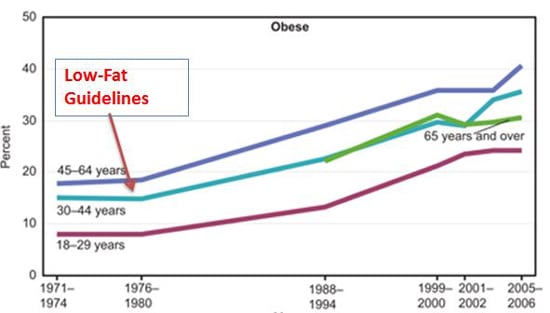
It is interesting – and a little infuriating – to note that climbing rates of obesity began with the advent of the low-fat craze. And opened the door for many new dangerous diet drugs – like Fen-Phen – to be prescribed to all the suddenly obese people.
The social, emotional and physical impact
I am old enough to remember being weighed in elementary school in front of all my classmates. A de-humanizing situation that no child should be put through. I have also cringed in a doctor’s office in my 20’s when the BMI chart came out and the finger wagging began. I was a comfy size M, fit enough to do aerobics classes 5 times a week and yet my BMI bestowed the label of obese on me. And so the diet rollercoaster began.
In my coaching practice, nearly every woman and a good portion of the men who come to me for support have been subjected to the BMI yardstick. Everyone of them have emotional scars about the embarrassment and shame it caused them. Several report that real and pressing medical issues were brushed off because they were deemed obese and told that their symptoms would go away if they just lost weight and brought their BMIs down. And not a one of them truly understood what the BMI was telling them about their health – except that they had to “eat less and move more”.
Not surprising – because all it is really telling them is that if you were an Amazon package, this is the size of box you’d need to accommodate your mass.
I’m truly not making light of this. Honestly, I’m damn mad about the continued myth that the BMI is the standard by which we measure our health. And by extension – our worth.
It’s dangerous and it’s demoralizing. Too many fitness trainers and physicians and dieticians and TV makeover shows are guilty of doing this and it’s got to stop.
At best, the BMI misleads White people about their weight and its relation to health. At worst, it precludes people of colour and people from diverse cultures from having any chance at all of being seen and having their health and weight story clearly understood.
So what’s the real measure of health?
Let’s put aside the BMI and consider other, more relevant ways to gauge how we’re doing in getting and staying healthy.
- Metabolic markers like blood sugar levels, insulin resistance, triglycerides and other blood lipids, heart rates, hormone levels, inflammation are all more likely to paint a more accurate picture as to whether someone is in good health or not than what their BMI number is, regardless of what they weigh. Get your tests done and know what the numbers mean.
- Measuring your body composition to understand the ratio and the levels of adipose (fat) tissue to lean tissue can tell a lot. Fun fact: Muhammed Ali, the heavyweight boxing champion of the world, was considered obese on the BMI chart because of his solid muscular build was, well, heavy. There are many scales available now for use at home to do these if your nutritionist does not have one (I do and I use it with my clients all the time).
- Your waist to hip ratio is very telling in terms of where you carry extra weight and whether that extra weight might be a risk. Abdominal fat is the riskiest – even if your BMI is in the normal range.
- Sleep cycles and stress responses, whether someone lives on processed foods and coffee, or eats vegetables and gets enough fibre and water, and moves their body joyfully each day are also important and relevant measures of overall health.
All of these factors and biomarkers are far more important than a mathematical equation. We have to do better and we can start by ignoring the BMI label we may have been given and focusing on the bigger picture of holistic health.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4890841/
https://www.scientificamerican.com/article/is-bmi-an-accurate-way-to-measure-body-fat/
https://elemental.medium.com/the-bizarre-and-racist-history-of-the-bmi-7d8dc2aa33bb
https://www.diabetes.co.uk/in-depth/fat-politics-nina-teicholz-seven-countries-study-dietary-policy/
https://thefemedic.com/news/why-bmi-indicator-health-dangerous/
https://www.scientificamerican.com/article/what-biomarkers-say-about-health/
